Courses
Our complete library of CE and CME accredited trainings for health professionals, such as physicians, program directors, psychologists, social workers, counselors, and other mental health clinicians and community workers.
Bundles
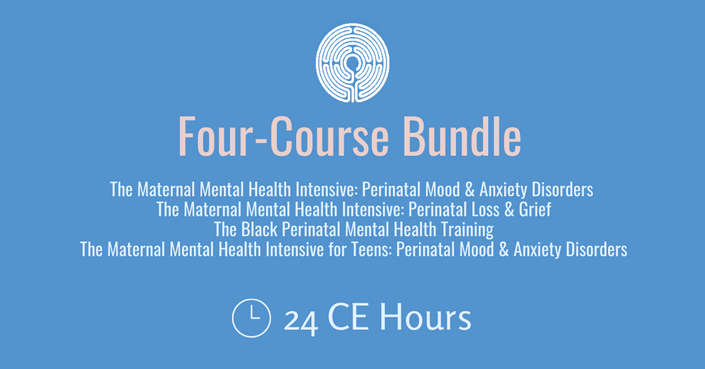
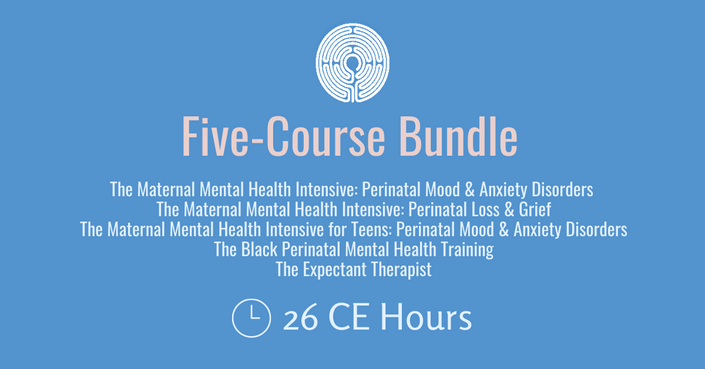
Our discounted Bundles combine multiple trainings at a reduced price.
Why You Should Train with Seleni
Have you ever seen a client post-pregnancy, and had difficulty determining whether they have the common baby blues, or a diagnosable mental health disorder?
Do you feel less confident treating new parents and those who are dealing with reproductive challenges such as IVF, adoption, and perinatal loss, and want to become more skilled in these areas?
Are you interested in learning this and more from multidisciplinary experts in the field who specialize in these topics in their own clinical practice?
As a mental health professional, it's likely you'll treat clients who face one or more of these challenges during their reproductive years, and who need specialized treatment to cope and move forward successfully.
Most graduate and professional training programs do not prepare professionals to support clients through these common challenges or provide in-depth exploration of other topics (such as infertility and miscarriage) that deeply impact the emotional wellbeing of even more women and families. To address this need, Seleni created the Maternal Mental Health Intensive, a 16-hour professional training which equips clinicians with critical, evidence-based tools to fully support clients through one of the most challenging times of their lives.
The Issues
Perinatal mood and anxiety disorders (PMADs) are among the most common pregnancy complications. They affect as many as 1 in 5 women – more than twice the number of women who develop gestational diabetes. Here are the facts:
- Up to 20% of women experience prenatal or postpartum depression, and postpartum anxiety affects 20% of first-time moms.
- 10-15% of women experience depression during pregnancy, but it often goes untreated.
- Women with infertility can feel as anxious or depressed as those diagnosed with cancer.
- Half of women experience significant distress following a miscarriage.
- Also, 1 in 4 pregnancies end in miscarriage, and 1 in 160 babies are stillborn.
Miscarriage and stillbirth are profound losses that are rarely talked about and little understood. Why? In our society, we have almost no understanding of how those who experience reproductive loss grieve and recover. Here are the facts:
- 1 in 4 pregnancies end in miscarriage; 1 in 160 pregnancies result in stillbirth.
- Women with a previous perinatal loss are at a high risk of experiencing perinatal depression and anxiety during subsequent pregnancies.
- One-third of women who suffer recurrent miscarriages will experience clinical depression.
Child loss can severely impair family functioning, negatively impacting generations to come. Women and their partners are often isolated in their grief and unsure of how to manage and move forward. One study found that parental bereavement was related to an 80% increase in suicide risk.
Unresolved grief from reproductive loss and child loss puts women at high risk for experiencing complicated grief and is a significant risk factor for developing a perinatal mood or anxiety disorder (PMAD).
Who should take our courses?
Seleni's trainings were created for professionals who work in healthcare and community spaces and seek empathetic, critical, and evidence-based training in build a knowledge base and skill set to serve clients facing reproductive mental health challenges. Our growing community of students and alums are dedicated to our shared mission to treat, support, and advocate for the emotional health of individuals and their families during the family-building years. They include psychologists, social workers, mental health counselors, students, doulas, and many more.
Are you looking to complete PSI's Perinatal Mental Health Certification?
Seleni’s 16-hour Maternal Mental Health Intensive Online Bundle Training is approved by PSI as an alternate pre-requisite training in the 3-step Certification in Perinatal Mental Health (PMH-C). All our 2-hour courses are approved by PSI to keep the PMH-C current by completing 12 CE hours every 2 years.
Discounts
Full-time students currently enrolled in an accredited graduate mental health program are eligible for a 25% discount. Discount is subject to proof of enrollment. Group rates for mental health professionals:
- 2-5 participants: 15%
- 6-9 participants: 20%
- 10+ participants: 25%
Please fill out this form to receive your personalized coupon, and if you are part of a larger organization, please submit the form and we'll reach back to you to discuss a further discount.
Only one discount code may be applied per order.
Continuing Education
Social workers, counselors, psychologists, doulas, and other professionals can earn continuing education credits with Seleni! Accreditation eligibility can be found on each course's page.